Partnering with Clinicians to Transform the Nursing Preceptorship Experience
- Dawn Goldstein, Ph.D., RN, PMHNP-BC
- Assistant Professor
- Director, Psychiatric Mental Health Nurse Practitioner Program
- College of Nursing
Project Overview
- Most faculty and clinicians who develop preceptorships for graduate nursing students have mastered the basics of transitioning the clinical experience from face-to-face to an online environment.
- What's missing is experiential, interactive learning curriculum that takes full advantage of the online platform's capabilities while minimizing its disadvantages.
- This project aims to close that gap.
Why This Work Matters
- Even before the onset of COVID-19, the replacement of face-to-face office visits with telehealth sessions was becoming the norm, especially for patients who live in remote areas. This form of health care delivery will not disappear anytime soon, even after the pandemic goes away. Developing its capabilities now will have far-reaching benefits into the future.
Products/Outcomes
- Experiential, interactive curriculum that is capable of providing many of the same learning outcomes as a face-to-face preceptorship
- More access to health care services and analysis of barriers to service for patients who use telehealth
- More effective, efficient, and economical use of health care providers' time
External Partners
- Margaret Keeler, Psychiatric Mental Health Nurse Practitioner, Lansing Institute of Behavioral Medicine
- Tamara Zurakowski, Ph.D., GNP-BC, Clinical Associate Professor, Virginia Commonwealth University, School of Nursing
- Numerous outpatient clinics in Michigan
MSU Collaborators
- Kimberly Krummrey, DNP, RN, FNP-C; student, Psychiatric Mental Health Nurse Practitioner Certification Program
- Psychiatric Mental Health Nurse Practitioner Certification Program
Form(s) of Engagement
- Community-Engaged Teaching and Learning
- Community-Engaged Service and Practice
- Clinical Practice
- Human and Animal Patient Care

Dawn Goldstein directs the Psychiatric Mental Health Nurse Practitioner (PMHNP) program at MSU's College of Nursing.
In the early spring of 2020, Dawn Goldstein was happily absorbed in connecting with clinics and hospitals, setting up placement opportunities for students in the MSU College of Nursing's Psychiatric Mental Health Nurse Practitioner program. Goldstein is the program director and an assistant professor in the College.
Then COVID-19 hit, swiftly followed by near-total lockdown. Goldstein's problems were more urgent than some. Because clinical placements involve close contact onsite with both patients and medical staff, many important decisions had to be made on the spot. Some students who had already started their placements were sent home and told not to return. Clinical partners who had initially agreed to sponsor a student backed out over the summer.
In response to the COVID-19-pandemic, with the sudden relaxing of regulations and unprecedented insurance support, clinicians have been enabled across a variety of settings to adopt telehealth services. At Lansing Institute of Behavioral Medicine, a designated clinical site for MSU College of Nursing, we rapidly converted outpatient services over to telepsychiatry, becoming fully operational in March 2020. In this large practice, which schedules over 900 patient visits per week, meeting the challenge required significant coordination between office and clinical staff.
For MSU College of Nursing student scholars, the experience has been gratifying and rich, while posing some challenges. The advantages of telepsychiatry include making it possible for the students to continue with their clinical experience, ease of asking the patient if the student can join the meeting, ease of scheduling patients back with the student, and allowance for keeping a brisk pace of seeing patients with a wide variety of psychiatric disorders for medication evaluation. Disadvantages include challenges of learning to provide add-on psychotherapy, such as the use of silence as an effective intervention tool and reading nonverbal communications (subtle changes in tone of voice, inflection, affect and gaze), which are so important in the learning experience. Overall, the experience has been educational and positive.
Ms. Margaret Keeler, PMHNP
Psychiatric Mental Health Nurse Practitioner
Dr. Roy Meland, D.O.
Psychiatrist and co-owner of LIOBM
Shifting to the Long-Term View
The quandary then became how to continue. "We had to get creative with how we taught different skills to students, using technology to mimic the live placement experience," Goldstein said. But Zoom was not a one-size-fits-all solution; it might be possible to provide some semblance of normal student-patient interaction in a clinical setting virtually, but not in a hospital. Besides, hospitals had problems of their own.
For Goldstein, not being able to drive out to meet potential partners and talk about the program was a real handicap. "You're trying to call people who are no longer in their office. You're trying to e-mail them, and they don't know who you are. So, I had a very poor response rate all through spring and summer," she said.
Life was not easy for the students, either. "Especially in the spring, our students really suffered," Goldstein said. Her program is a graduate program, and all the students in it are working nurses. Many of them who ended up working in COVID units were asked to put in extra hours. Others were furloughed when their facility turned into a COVID facility and they had to go somewhere else or reduce their hours.
After weathering the initial shock and scrambling to put temporary solutions in place, faculty and administrators across the University began turning their attention to the long view. It had become obvious that (1) the pandemic was not going away anytime soon, and (2), as Goldstein said, "You can't just take a face-to-face class and plop it into an online platform; you have to take the time to build and develop an interactive curriculum."
Health Care Delivery is Changing
Even before the impact of COVID, the delivery of health care has been quietly changing for some time.
Telehealth is coming into its own as a communication option for any number of reasons. It is especially a boon to remote rural areas that previously had very few medical services available. Patients who have mobility or transportation issues love it. But there are problems, some related to the medium itself and some related to the circumstances of the pandemic.
Before COVID, patients would come into their local clinic and have a telehealth session with a specialist, usually someone from outside. The clinic would set up the session and make sure that everybody who needed to be signed on was ready and the technology was working.
Now face-to-face contact between patients and clinicians is discouraged and patients are expected to do their sessions at home.
"This means they have to build an infrastructure of how to do telehealth from someone's home," Goldstein said. "And you can't get a patient's vital signs, you can't do a lot of things that you used to do before you sat down and talked with them. Then you have struggle with the patient's Internet connectivity. Do they have the technology at home? It's one thing for them to come into the clinic and get set up for a telehealth encounter, it's another thing for them to do it by themselves. They may have their session in the kitchen with other family members present and listening in on the appointment. It's not very private. They may not have accessibility to reliable Internet or have adequate bandwidth. They may not have a laptop, so they're using their smartphone. So—a lot of barriers, but at least they're being seen."
A patient talks to a therapist during a telehealth meeting. Telepsychiatry is fast becoming a norm of psychiatric practice.
For Clinical Faculty, Institutional Support Makes a Big Difference
Goldstein has only good things to say about the supports her college and other departments have offered to help faculty navigate the transition to the online platform. "I applaud the departments for these efforts," she said. "You're with other faculty, from different colleges, in synchronous webinars, and you're working on problem solving with those people. It's helpful to see what they're doing and what's working."
She took a writing workshop about how to assist and evaluate her students with writing in the virtual environment. Normally her students would have gone for a monthly simulation at the Collaborative Learning Center, but now all those simulations are virtual. Instead, they are learning to build their own virtual scenario as though a patient is coming into a clinic or being seen at home. These skills help them prepare for conducting a psychiatric evaluation or follow-up via telehealth. Although the exercise is being done out of necessity, Goldstein believes that in this case, that's not a bad thing: "Telehealth is a good skill that they've had to learn."
Honing Skills for Online Learning Environments
Goldstein is excited about "honing our skills on how we deliver content online, making it meaningful and understanding that you can't just throw an hour-long lecture online for students to listen to—but how do we tailor what we deliver? How do we help students be more engaged?" She sees technology as playing a major role but wonders how it can be utilized better.
Dr. Dawn Goldstein was my faculty advisor for completing my doctorate in nursing practice (DNP). Her guidance has helped me become a stronger scholar and clinician in my current role as nurse practitioner at MSU Pediatric Pulmonary. I have learned how to conduct research and perform quality improvement projects to implement evidence-based practice for patient care.
I am one of six in the first cohort enrolled in the post-master's Psychiatric Mental Health Nurse Practitioner (PMHNP) certification program at MSU. I am learning how to conduct a psychiatric evaluation, assessment, diagnosis, and treatment plan for individuals with mental health issues. The program also includes learning psychotherapy techniques to reinforce coping and behavioral training to augment medication management.
My clinical site is at Lansing Institute of Behavioral Medicine (LIBM) with Margaret Keeler, PMHNP. Margaret has been a stellar preceptor, allowing me to use my interviewing skills and help formulate a plan of care. She has included me in mental health community events and allows me time to ask questions and review clinical cases. She has supported me to work from home via telehealth during the pandemic, which allows me extra time to care for my two children. Margaret is also a mental health advocate in the Lansing community, which has allowed me insight to the mental health barriers at the local and state levels.
Kimberly Krummrey, DNP, RN, FNP-C
Student, Psychiatric Mental Health Nurse Practitioner Certification Program
Care Coordinator, PIONEER Program at LIBM
"I don't think that my students will be able to see patients face-to-face unless they go on an inpatient setting," she said. "And then it'll be wearing the masks, the goggles, a face shield, whatever PPE they need. And there's the risk—I walked around a psychiatric unit about a month ago and noticed that the staff was all wearing PPE, but none of the patients were. Students must be worried about who they're sitting down with for an hour. Technology is going to have to take a much more active role."
Beyond COVID: Moving Clinical Nursing Preceptorships Online
Some clinics are still seeing patients face-to-face; most are not. Telehealth has become the norm, but not all are ready to bring back the students, even virtually. Clinical preceptors as well as faculty mentors have to understand how to create online experiences that advance student learning as well as train them in the basic process of conducting therapy sessions online.
Primary care Improved Outcomes with Nurses in Evolving and Expanding Roles (PIONEER) is a federal Health Resources and Services Administration (HRSA) grant based at Virginia Commonwealth University. Tamara Zurakowski, clinical associate professor at the VCU School of Nursing, is principal investigator; Goldstein is a co-investigator for this four-year sub-grant of the project. Numerous clinical partners are involved.
PIONEER aims to design and deliver education in primary care nursing to senior nursing students, educate and support the clinical partners' RNs in their enhanced role in primary care, and assist clinical partners in adopting primary care practices from the LEAP project, which is housed at VCU's Center for Disability Leadership. LEAP clinics emphasize team-based care, enhanced roles for MAs and RNs, layperson involvement, complex illness management, behavioral health integration, and clinic-community connections.
The MSU team's role in this larger picture is to provide the training. "HRSA was generous to give additional monies to all the recipients of the grant to help us develop telehealth education, certification for our clinical partners, and supplies like peripherals," Goldstein said. "Some clinics were also interested in electronic devices that can be given to patients in the home, such as iPads or peripheral devices, e.g., dual ECG and digital stethoscope, or electronic blood pressure monitor device."

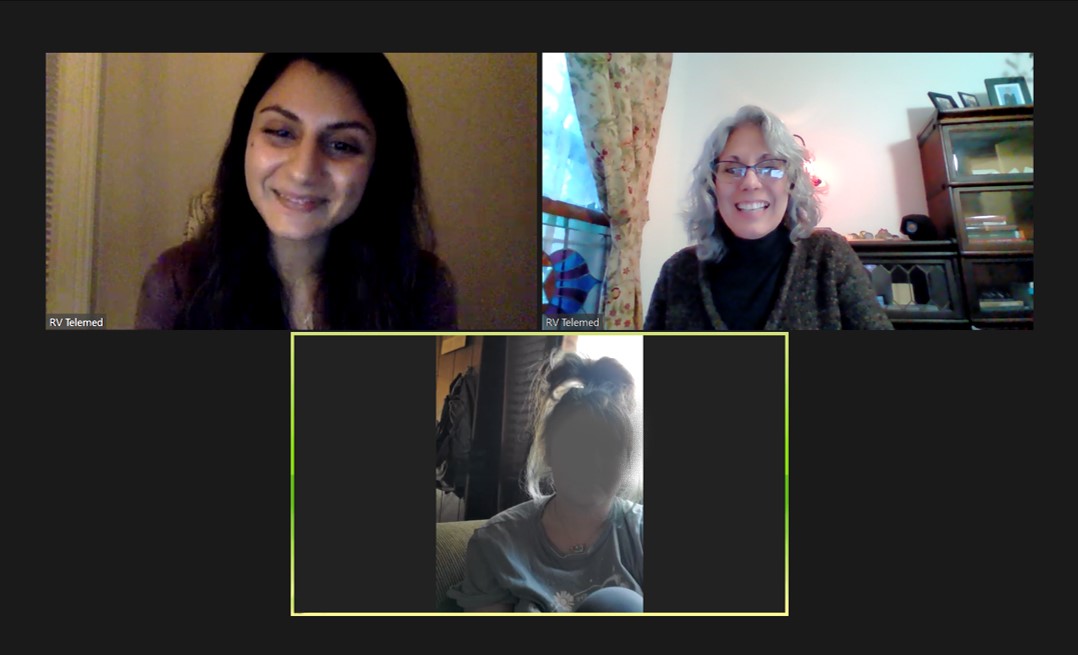
Margaret Keeler (on left) is a psychiatric mental health nurse practitioner at the Lansing Institute of Behavioral Medicine, a designated clinical site for MSU's College of Nursing. Kim Krummrey (on right) is one of six in the first cohort to be enrolled in the College's post-master's PMHNP certification program. Keeler is Krummrey's clinical preceptor. Dr. Goldstein was Krummrey's faculty advisor for completing her doctorate in nursing practice.
Goldstein's future plans include a new grant proposal to be submitted in January, looking at a few primary care clinics in the Upper Peninsula and providing them with an online source of education to train their staff in behavioral health with a focus on children, adolescents, and transitioning adolescents.
Integrating behavioral health and primary care is her first goal. She plans to enlist faculty from at least two different disciplines within MSU; she is particularly interested in partnering with the Department of Psychiatry, along with the College of Nursing's psychiatric nursing and psychiatric mental health nurse practitioner programs, to deliver care, education for these clinics, and telehealth.
Advice for Navigating the Post-COVID World
Goldstein advises fellow travelers to take advantage of every educational opportunity they can get: "When your college offers these educational opportunities to learn how to do the translation of your curriculum from a face-to-face to an online environment, you're looking at the people who have that expertise. Take up that opportunity. Take advantage of it to learn and integrate it into your curriculum. Even though I've been teaching online, I found it invaluable."
She has been thinking about developing an educational video to help her partners understand that they can still precept a student and see a patient via telehealth, "because that was such a barrier for some clinics they thought 'Nope, we can't have your students because we're doing this.' But it really is possible, because I've been doing it. And it does work and some of my other students are with other clinical partners. They're seeing patients via telehealth as well. I don't see that going away."
- Written by Linda Chapel Jackson, University Outreach and Engagement
- Photographs courtesy of MSU Counseling and Psychiatric Services (top), Dawn Goldstein, and Paul Phipps (bottom), University Outreach and Engagement